As Kate Hendricks Thomas sat one night with her second-grade son Matthew, he placed his hands on the table as if he were an adult girding up for an important conversation.
“Mom,” Kate remembers him saying, “I’m not going to cry when I say this.”
And then, she says, he started to cry, but just a little bit. Her heart tightened in her chest as she waited.
“He said, ‘I just want you to know, when you die, I’m going to cry so hard because I love you so much,’” she remembers.
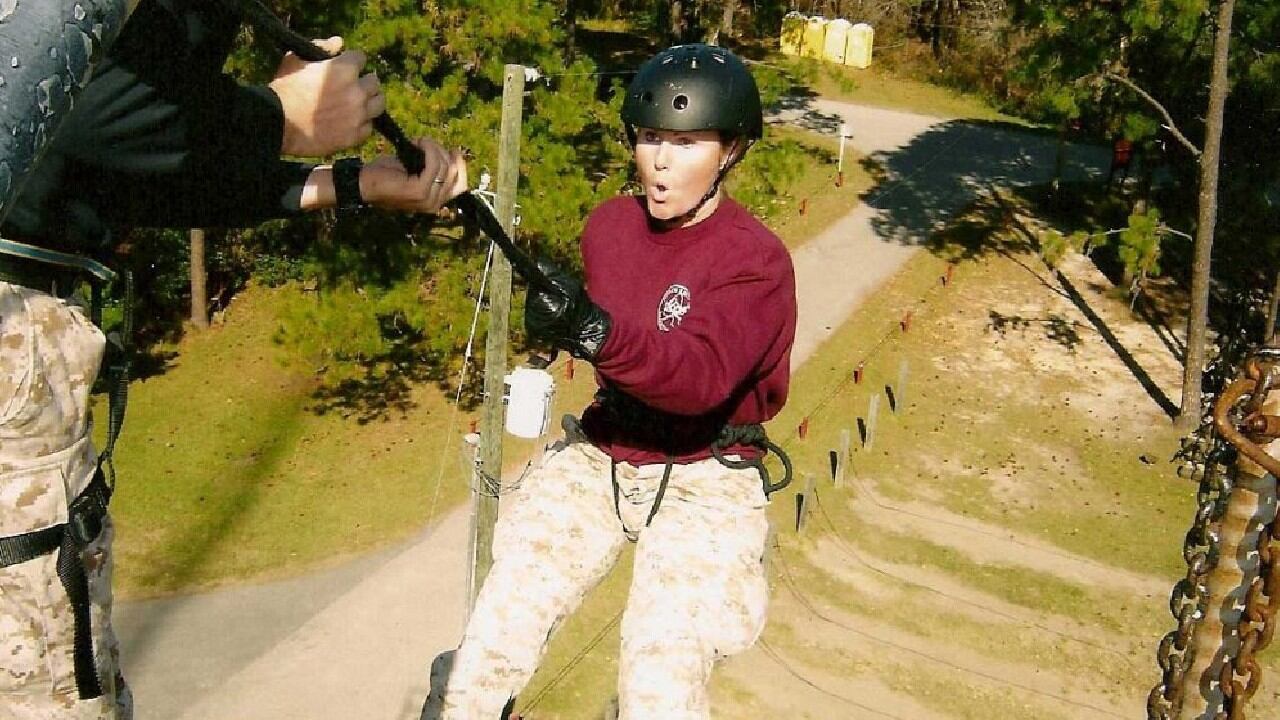
Hendricks Thomas shines fiercely: A former Marine Corps officer, she hit Fallujah, Iraq, in 2005, when the living was still dirty and the second battle of Fallujah had just reached its end. To stay healthy, she ran laps around the burn pit on base. After she got out of the military, she earned her doctorate — and a reputation for helping others through the hard stuff.
She mastered resiliency, co-writing a book about it and urging community, mindfulness, and physical health as she saw fellow service members and veterans struggle with combat stress. She gathers friends in close and offers praise and insight in large doses.
One day in 2018, in the middle of interviews and speeches about the books she had co-written, she went in for her annual gynecology exam.
“I was feeling great,” she says. “I had no symptoms. I was there for an annual appointment.”
Her nurse practitioner recommended she get a mammogram, “based on where you’ve been stationed.”
“It was totally out of the blue,” Hendricks Thomas says. “And that’s why I argued with her about it.”
She was 38. It was already stage four. And she doesn’t have one kind of cancer: She has three.
She has no family history of breast cancer, and when they looked for predictor proteins — ”next generation sequencing” — she had no indicators. Worse, as she started talking with another Marine who served in her unit, Amy Ebitz, she learned Ebitz also had breast cancer, that it was also invasive, and that she also had no genetic markers.
“Somehow the topic of breast cancer came up, and we were both very surprised — very surprised,” she says. “Her physician said this is very likely an exposure-based cancer. And that’s what my oncologist said to me when the sequencing came back.”
Ebitz had served at Fallujah, but also says she lived half a mile away from the burn pit at al-Taqqadum in 2004. She started to become suspicious when two men from her unit were diagnosed with cancer, but before that, she wondered if something was going on when the working dogs in her unit started to get sick.
“The first tour, it was no big deal — we dealt with paw issues,” she says. “By the second tour, we kept losing dogs to cancer — three-year-olds. I remember the kennel master saying, ‘How long do you think before this will start on us?’”
Ebitz got a mammogram when she turned 40, and she was told it was clear. But she had a bad feeling. There were no lumps, but she felt “draggy.”
“I can’t explain it,” she says. “I didn’t have any symptoms. But I said to my battalion surgeon, ‘Something’s wrong with me.’”
Two years after the clear mammogram, she had more tests done. She had stage two cancer — and it was “just like Kate’s.”
“I had a seven-year-old son,” she says, and her daughter was three. “I was terrified.”
At that point, she said she thought it was a coincidence. Then she started thinking about a male major she had worked with who had breast cancer, and a male commanding officer who also had it.
“When I was going through treatment, the provost called and said one of his guys had non-Hodgkin’s lymphoma,” she says. She began to wonder if they had all been exposed to something in Iraq.
For both Hendricks Thomas and Ebitz, their breast cancer was heterogeneous and moved quickly, which Hendricks Thomas says caused her doctor to suspect a toxic exposure. Her doctor also said she had been seeing more of it in military women.
“It was a fluke that she sent me out for that mammogram,” Hendricks Thomas says. “I mean, they wouldn’t have found this cancer until it kills me. She added years to my life by sending me out for screening. And I actually became a proselytizer and told all of my veteran girlfriends, ‘Please go get mammograms.’”
Ebitz, who served as battalion executive officer in Fallujah, said she didn’t talk about it at first — she didn’t want her Marines to know she’d had breast cancer. But then people started asking about her hair loss, and she decided to spread the word.
“Now that I’m a few years out, I tell everybody: ‘Get it checked,’” she says. “The enemy is lurking in our bodies.”
A push for testing and benefits
Numbers for breast cancer in military women have been high for years, but as veterans returned from the wars in Iraq and Afghanistan, rumors began to swirl: The cancers are hitting young—and they’re extraordinarily aggressive.
From fiscal year 2000 to fiscal year 2015, Veterans Affairs saw the number of women diagnosed with breast cancer increase by five times for women ages 45 to 64 — or 3 percent of Veterans Health Administration patients in this age group — by fiscal year 2015, according to a VA report.
Authors said the increase could come because of better screening, or it could be a “true increase in prevalence.”
And a 2021 VA-funded research proposal by Rajeev Samant states this: “There is a notably high incidence of breast cancer among younger military women (20 percent to 40 percent higher). The incident rate of breast cancer for active-duty women is seven times higher than the average incident rate of 15 other cancer types across all service members. An estimated 90 percent of deaths due to breast cancer are a consequence of metastatic disease. Thus, metastasis is a formidable and clearly an unmet challenge.”
These young women are dying.
“Thus, there is an urgent unmet need to effectively diagnose, manage and cure breast cancer in the veteran population,” Samant’s proposal states. “Triple-negative breast cancer (TNBC) is prevalent among young women veterans, and shows a tendency to rapidly metastasize. Despite a short favorable management with chemotherapy, patients with metastatic disease have a median overall survival of about 18 months.”
As the last troops leave the “forever wars,” doctors say they’re seeing more women veterans with breast cancer — and they’re younger than the national average. This is of particular concern because doctors don’t tell women to get mammograms until they are 45, unless they have a family history of breast cancer.

Generally speaking, service members tend to have lower rates of all cancer compared to the civilian population, in part because they need to be fit for their jobs and they have access to healthcare. The new cancers are rare and aggressive, and the medical system built to help veterans simply isn’t equipped to handle breast cancer in young women, activists say.
So, some doctors and the women veterans themselves are pushing young women to get checked — and researchers are starting to look more deeply into environmental factors as a cause for aggressive, nonhereditary breast cancers whose growth is not driven by hormones. In the meantime, activists, like Hendricks Thomas, and politicians are pushing for service-connected VA benefits for women.
There have been some breakthroughs: VA says the rates may be higher because of better screening, higher rates of aggressive breast cancer in women in minority groups may get research attention that has lacked for generations, and a push to predict and treat breast cancer in military and veteran women could help other women around the world.
‘It’s gotten around every drug we’ve thrown at it’
When Hendricks Thomas was diagnosed, she faced an immediate concern: She served as the breadwinner in her family, and she would need some help. Her first claim for service-connected benefits at VA was denied.
She filed an appeal.
Denied.
This meant no survivors benefits for her son, and no help for her family in paying for her treatment. Her resiliency and strength once again came through: She began to fight for the Presumptive Benefits for War Fighters Exposed to Burn Pits and Other Toxins Act, which would provide presumptive benefits for veterans exposed to the burn pits — and which was lobbied for by talk show host Jon Stewart and John Feal, a 9/11 first responder who formed the FealGood Foundation. In August, VA announced it would assign presumptive status for some respiratory ailments.
The change helps, as might the burn pit bill, but neither addresses breast cancer.
So it’s not enough for Hendricks Thomas. Beyond benefits, she wants to save lives.
She calls herself a “fangirl” of a VA oncologist she met at a conference, Anita Aggarwal of the Washington DC VA Medical Center, but adds, “She says she has young women coming into her office with this advanced breast cancer, this aggressive, advanced breast cancer. Mine is still heterogeneous” — resistant to treatment. “It’s gotten around every drug we’ve thrown at it in a matter of months, because it keeps morphing. And she said, ‘You know, that’s weird. That’s atypical, and I’m seeing lots of young women with that sort of thing happening.’”
The more she talks to others about her cancer, the more stories she hears: She recently met a woman younger than 30 who has both breast and colon cancer. She knows two women still on active duty with aggressive cancers, she says, and four veterans.
“I don’t understand why we haven’t lowered the screening age for military women,” she says. “I know it’s early, but ask your providers.” Women are often told by their primary care physicians at VA that they don’t need a mammogram yet, she says, and that there’s no additional risk. “So the VA is not even doing the preventive bare minimum. I mean, if all they were willing to do was lower the screening age, that would be a step forward.”
Military health care covers annual mammograms for women older than 40 or women 30 and over who are at high risk of developing breast cancer. Many Defense Department facilities have breast high-risk programs or breast genetics programs to help identify high-risk patients and screen them early, Defense Health Agency officials said in an email.

VA recommends that all women between age 50 and age 75 get mammograms every two years, but also that women have mammograms after age 40 if they choose to. However, VA does not perform mammograms in 15 states. A new bill hopes to address that.
“VA exceeds the private sector in mammography screening rates,” VA spokesperson Terrence Hayes said in an email, adding that VA’s rate of screening for women ages 50 to 74 is about 84 percent, compared to civilian HMO rates of about 74 percent in 2018.
“Like other health care agencies, we have seen some delays in routine screening related to COVID, but we are addressing this challenge by using a Preventive Health Inventory to ensure all our patients are up to date on all preventive screenings,” he says.
But VA officials say they don’t yet have data to support the women veterans’ fears.
“VA acknowledges recent individual reports of post-911 women veterans being diagnosed with breast cancer,” Hayes says. “We are following this issue closely. However, to date we have no research to support higher rates of breast cancer in post-911 women veterans following deployment.”
Hayes said Congress directed the Defense Department to look at the rate of breast cancer in active-duty women, and he quoted the abstract from that report, which says, “The findings from this study indicated that breast cancer among active service members is a rare event.” The abstract states that the breast cancer incidence rate from 2000 to 2010 did not change significantly.
The activists say that makes sense. As Stewart and Feal lobbied for first responders to the World Trade Center attacks in 2011, they learned service members were likely exposed to the same kinds of chemicals in the burn pits in Iraq and Afghanistan, they told The War Horse. Because the first responders were exposed to toxins before service members were exposed to the burn pits, Stewart and Feal said they expected some of the same patterns to emerge.
According to a CDC report released in September, 58 percent of people who signed up for the World Trade Center Health Program have reported at least one illness caused by exposure, and cancers had risen by more than 1,000 percent from 2013 to 2020.
In 2020, the top five certified cancer conditions were skin cancer, male genital system cancers, in situ neoplasms, breast cancer, and digestive system cancers, according to the report.
“The problem with cancer — with all of the cancers — is that you often deal with the delayed onset, as you know,” Hendricks Thomas says. Breathing problems or skin rashes from exposure often arise immediately. Cancer can take years. “So it’s easier to be dismissive of those.”

The number of women in general, both civilian and military, diagnosed with breast cancer has increased — from 1 in 11 in 1975 to 1 in eight today — with the median age for diagnosis at 63 for white women and 60 for Black women. But active-duty military women have a 20 percent to 40 percent higher risk than do civilians, a 2009 study published by the National Institutes of Health found — and 90 percent of military women are younger than 40, according to the Defense Department’s Congressionally Directed Medical Research Program.
Younger women diagnosed with breast cancer have higher mortality rates.
In 2018, researchers looked at breast cancer in the Defense Department’s database. Typically, only 7 percent of breast cancer cases affect women younger than 40. But from 1998 to 2007, the researchers found 11 percent of diagnosed military cases were in women younger than 40. Their cancers tended to be later stage, and they also tended to be estrogen-receptor negative — like Hendricks Thomas and Ebitz.
According to the National Institute of Environmental Health Sciences, evidence is growing to support the idea that many breast cancers are caused by environmental factors, including a 2017 study of sisters that found that indoor wood-burning fireplaces or stoves were associated with a higher risk of breast cancer.
A 2004 study published in the European Journal of Cancer Prevention found higher rates of breast cancer in women with a specific gene who had been exposed to a waste incinerator that, like the burn pits in Iraq and Afghanistan, would have released dioxins, as well as being exposed to agricultural products, such as pesticides and dioxin-like compounds.
In another 2018 study of women enrolled in the Clinical Breast Care Project at Walter Reed National Military Medical Center, researchers found “significantly” different levels of organochlorine levels — or synthetic pesticides — depending on the stage of the cancer and grade of the cancer, and whether it was hormone-positive, “indicating that the body burden of organochlorines may influence the development of specific subtypes of breast cancer.”
Organochlorines are also used in dry-cleaning solvents, adhesives, lubricants, and hydraulic fluids. The burn pits in Iraq and Afghanistan released dioxin, an organochlorine released as a by-product of burning waste. The largest open burn pit, at Balad Air Base, devoured as much as 240 tons of trash a day within one mile of the living quarters of troops.
Women who deployed to Iraq and Afghanistan, or anywhere the water source was considered risky, also drank water from plastic bottles. In Iraq and Afghanistan, those bottles often sat in the sun for hours. Research has shown that plastic that contains BPA may be associated with breast cancer.
And it’s not just women. Aggarwal found that breast cancer rates among male veterans have risen by 26 percent since 1975 — though they still remain low. The concern? Women are taught to do monthly breast exams on themselves. Men are not.
‘It was turned down twice’
Experts have long known there was an issue, and some of the reasons seem pretty obvious: A 2012 study found a 40 percent increased risk of breast cancer in women who work night shifts — as military women often do. And military women are more likely than civilian women to work in jobs, such as mechanic or fuel operator, that might expose them to volatile organic compounds. A 2005 study found that military women younger than 35 working with VOCs had a 48 percent increased risk of breast cancer. The military has also had problems with contamination on base. Marine Corps base Camp Lejeune had the metal degreaser trichloroethylene and a dry-cleaning chemical, tetrachloroethylene, in the water. Civilians who worked there between 1973-1985 had higher rates of all cancers compared to people who worked at Camp Pendleton. Another study “suggested possible associations” between male breast cancer and the Camp Lejeune water. And another study found military women are also more likely to use birth control — it’s easy to get and it’s free — which has been associated with an increased risk of breast cancer in young, premenopausal women.
There has been some work around the possibility that the burn pits, in particular, may be causing fast-growing cancers. Aggarwal, the oncologist Hendricks Thomas met at a conference, has submitted a proposal to the Defense Department looking at the connection between exposures and breast cancer to see if it might help account for the increased incidence of breast cancer in military women.
“Very little evidence is available linking toxic exposures to increased breast cancer risk in veterans,” she writes in her proposal. “Study of breast cancer incidence associated with military occupational assignments, deployments, or other service-related experiences is greatly constrained by the latency between exposure and onset of cancer, as well as the Department’s inability to conduct surveillance on most service members after they leave service.”
She hoped to compare women veterans who deployed to those who did not.
“It was turned down twice — very discouraging,” Aggarwal said in an email. She also talked to two Congress members to try to push the issue. They promised to get back, but she “never heard anything from them.”
None of it should be new to the Defense Department, Hendricks Thomas says.
“[Aggarwal] shared her background section of her grant with me, and those data are from Walter Reed,” she says. “This is stuff that the military already knows.”
Hendricks Thomas says Aggarwal is the only VA medical professional she found who was willing to be open about the issue. She asked the nurse practitioner who originally told her to get the mammogram if she would help with her VA disability claim, but says the woman said no — that she didn’t want to put it in writing.
‘Just sick with something’
Hereditary cancer can also hit military women early. Just before Jessica Brooks turned 40 in 2018, she went in for her annual exam. At the time, she was going to school to become a nurse practitioner while she was in the Air Force. She had never deployed. She mentioned at the appointment that she could feel a swollen lymph node in her armpit, but she figured she was “just sick with something.”
But the lump in her armpit was bigger than it should have been — ”It was the about the size of a golf ball,” she says, “and lymph nodes are typically about the size of your pinky” — and it was tender.
Soon after, she received a phone call saying she had cancer. She would ultimately learn it was stage three.
“I was like, ‘I’m young, what the heck?’” she says. “Nobody gets cancer this young.”
But in her case, while she didn’t have a strong history of breast cancer in her family beyond an 80-year-old grandmother, tests showed she did have a PALB2 mutation, she says. When her mother heard the news, she also went in — and her doctors found breast cancer, Brooks says.

As a service member, she says she had a choice between being seen at Walter Reed’s oncology center, or being seen locally. At the time, she lived in Maryland, so she went to the breast cancer center at Walter Reed.
“They are very well equipped to handle cancer,” she says. She now has a clean bill of health, and attributes that to good healthcare through the military.
Hendricks Thomas faced a different issue at VA in South Carolina.
“I didn’t go there, because they had only seen two women with breast cancer,” she says. “In D.C., I’m not able to quickly get scanned and quickly move things forward.”
She encountered a wait time for everything, she says, and she didn’t have time to wait.
“I needed a scan, and they said, ‘Great. We can fit you in in six weeks.’” With stage four cancer, a lot can happen in six weeks. She paid for civilian care, making her fight for benefits that much more important.
The House and Senate both introduced bills in July to help veterans access care by providing telemammography in states where VA doesn’t have mammograms, while also requiring VA to update those facilities within two years. The bills also require expanding veterans’ access to clinical trials.
Worse for minority women
There may be some good news in the mix: As the military studies service women, they look at women from all races. This is important because, in the civilian world, the death rate for Black women with breast cancer is 40 percent higher than the death rate for white women. It’s not much better in the military.
But the Defense Department is heavily involved in breast cancer research almost by default through the Defense Departments’ Congressionally Directed Medical Research Program. The program began in 1992 after breast cancer advocates pushed Congress to support high-impact, innovative research by the government. From that point on, Congress has funded the military’s Breast Cancer Research Program. In fiscal year 2021, the program received $150 million. The Uniformed Services University of the Health Sciences also has research programs.
A 2014 Defense Department report to Congress found that Black service women have a significantly higher probability of invasive breast cancer than do white and Hispanic active-duty service women. A 2019 study published in JAMA Surgery found that, from 1998 to 2008, Black women in the military health system waited longer for surgery after being diagnosed with breast cancer than did white women. But that still did not account for the disparity in overall survival rates, the authors wrote — and they urged further research.
“Treatment delays could lead to poorer treatment response, more rapid disease progression, or adverse health events and may contribute to reduced overall survival,” they wrote. They wondered why women who have access to health care in the military would still wait longer for treatment after being diagnosed with breast cancer. The Black women tended to be younger at diagnosis, were more likely to have stage II or III tumors and comorbid conditions, as well as more likely to have hormone-negative tumors, which means they can’t be treated by adjusting estrogen or progesterone levels. The majority — 70 percent to 80 percent — of breast tumors are hormone-positive, according to the Susan G. Komen foundation. Women with hormone-negative breast cancer are usually diagnosed at younger ages and are less likely to survive it.
The non-Hispanic Black women were more likely to have died during the study compared to non-Hispanic white women.
New research on veterans and service members may help address that issue.
In October 2020, VA announced it was launching a new National Women Veterans Oncology System of Excellence specifically to address women’s breast cancer.
About 700 women veterans a year are diagnosed with breast cancer, Hayes says.
As is often the case with health research surrounding veterans, environmental exposure statistics, as well as deeper research into minority women with cancer, may come to the forefront with new research.
One proposal comes as part of the Million Veterans Program, which now has 825,000 veterans signed up to offer information that can be used by researchers. Shiuh-Wen Luoh, of the Portland VA Medical Center, writes in a research proposal that 28 percent of the women in that group are Black, while past studies on genetic prediction models have typically been on white women.
“Our work will significantly enhance our abilities for early detection and optimize and individualize breast cancer screening for all women veterans and women in general,” he writes in his proposal. “Because women veterans in [the Million Veteran Program] may have unique military and environmental exposures, it is unknown whether previously developed breast cancer risk prediction models can be applied to this population,” the proposal states.
VA officials sent The War Horse a list of 27 current research projects that mainly focus on treatments and predicting breast cancer based on genetics.
‘As normal a life as possible’
There have already been some breakthroughs.
In August, researchers figured out how to use deep machine learning for biomarker analysis to help detect and treat breast cancer — and it came about because of an ongoing collaboration among Google Health, Naval Medical Center San Diego, and the Henry M. Jackson Foundation for the Advancement of Military Medicine.
Also in August, research through VA’s Million Veteran Program found that, by looking at DNA, a genetic risk model could predict which people are at the highest risk to get breast cancer. Doctors could use this information to help women figure out how often to be screened and if there are other steps they need to take to prevent breast cancer.
A third study, published in August in Cancer Cell International, found that one new breast cancer vaccine may be helpful in battling cancer, while a second appears to create a strong immune response.
But Hendricks Thomas’s battle continues. She’s participated in clinical trials, and is hopeful for more, but each treatment eventually loses effectiveness. During another round of chemotherapy, she has again lost her hair. But she finds hope in the everyday.
“I’m trying to make good choices, because it’s just so hard,” she says. “Because if it was just me, I would stop treatment — I wouldn’t do this dance. It’s too much. And the drug side effects are too much. But I’ve always had to think of my son.”
After a flurry of treatments — each working for a bit, and then stopping — her activity was limited. She couldn’t travel to promote her books. She was too exhausted to keep her normal caseload.
“I miss the pace,” she says.
Still, she hangs onto her work as a piece of her identity, and she keeps her family close.
“I have to live as normal a life as possible and do the things that I know make a person able to balance,” she says. “Like right now, I’m in a particular period of lots of doctors’ appointments and lots of stress, and it’s easy to get dizzy, to get kind of down. So in those times, I know that I have to practice the self-care techniques that are going to regulate my nervous system.”
She’s been taking an online course in mindfulness. She’s working to be a good mother and a good partner. And she’s hopeful that her experience will help other women.
“I think it’s a pipe dream that the Rubio-Gillibrand bill would pass and I would actually get a disability rating,” she says. “That feels like a pipe dream. But if that happens, because of my advocacy work, that would be a huge blessing for my family.”
This summer, her VA claim was, in fact, approved, and she received full benefits for breast cancer related to toxic exposure, relieving some of the additional stress she faced.
And she goes to a support group for women veterans with cancer. Recently, the group’s caseworker spoke out in amazement: “‘You don’t want to talk about feelings,’” Hendricks Thomas remembers her saying. “‘You want to talk about what action you can take to move the ball forward on this issue.’ She basically call[s] us all weird. But the advocacy work has held me up in the last couple of months. I mean, writing and speaking, and just thinking about this has felt—I feel a sense of purpose with that. So that’s been nice.”
In the meantime, her son has started school with the normal flurry of backpacks and lunch pails and new pencils.
“He’s a little guy,” Hendricks Thomas says, and her smile goes wide. “He plays and he goes to school, and he keeps me grounded in the day-to-day and in the present moment. Because I have to be if I’m going to be with him.”
Kelly Kennedy is the Managing Editor for The War Horse. Kelly is a bestselling author and award-winning journalist who served in the U.S. Army from 1987 to 1993, including tours in the Middle East during Desert Storm, and in Mogadishu, Somalia. She has worked as a health policy reporter for USA TODAY, spent five years covering military health at Military Times, and is the author of “They Fought for Each Other: The Triumph and Tragedy of the Hardest Hit Unit in Iraq,” and the co-author of “Fight Like a Girl: The Truth About How Female Marines are Trained,” with Kate Germano. As a journalist, she was embedded in both Iraq and Afghanistan. She is the only U.S. female journalist to both serve in combat and cover it as a civilian journalist, and she is the first female president of Military Reporters and Editors.




